To investigate whether clinically important ethnic inequities between Māori and non-Māori exist within EDs across Aotearoa New Zealand.
The EEDI study hypothesises that:
Research objectives investigated ED inequities within:
The EEDI project was undertaken with a Kaupapa Māori Research (KMR) positioning.
KMR places Māori at the centre of enquiry in order to make a positive difference to Māori communities. The EEDI project reflects KMR through a range of practices:
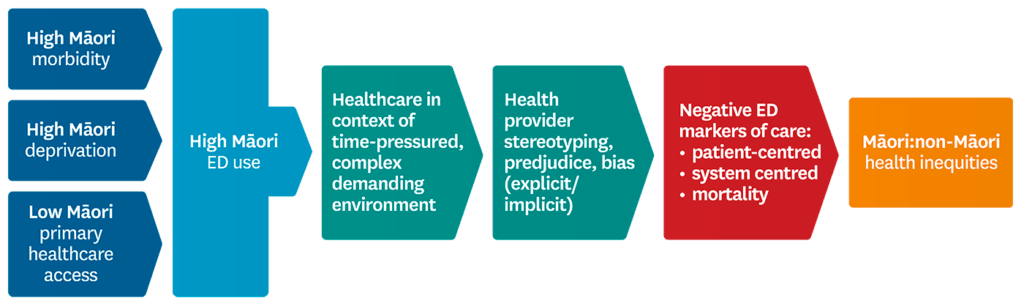
The diagram below illustrates the basic conceptual framework for EEDI that highlights high Māori ED use and the complex ED environment as precursors for potential provider bias leading to ethnic inequities in ED outcomes.
Ethical approval was obtained from the NZ Health and Disability Ethics Committee (HDEC 17/NTB/185).